Health system expansions can pose safety risks

Key takeaways
The Concern: Mergers, acquisitions and new affiliations among provider organizations cause changes that may put clinicians and patients at risk.
The Background: Health systems and hospitals have been growing through new partnerships, and data is lacking about how those deals affect the quality of care and patient safety.
Key takeaways
The Response: Harvard malpractice insurer CRICO and Ariadne Labs in Boston are studying the effects of health system expansion on patient safety and developing tools to help organizations plan for safe and successful clinical implementation.
The Action: Organizations, including Massachusetts General Hospital, are using a toolkit developed by CRICO and Ariadne to bolster their own efforts to understand the effects of new partnerships and to ensure patient safety.
When a Boston academic medical center shifted its total hip replacement cases to an affiliated community hospital, the transfer meant more than just busier operating rooms and higher surgical volume for its partner. The shift also meant the community hospital would likely see an uptick in emergency room visits, physical therapy cases and more. Might there be other unintended consequences?
Between 2010 and 2016, the number of U.S. health systems that expanded through new partnerships grew by 55 percent. As the anecdote above illustrates, the effects of expansion can be felt throughout the organization and may not be easy to anticipate. As mergers, acquisitions and new affiliations continue, organizations should consider the safety of clinicians and patients when they make plans that affect the delivery of care. How can hospitals best prepare to keep everyone safe and continue to provide high quality care during major transitions?
Large-scale mergers in Massachusetts
Massachusetts is part of a national trend. The Commonwealth saw 10 or more merger applications in both 2016 and 2017. And, this year, one huge merger of 13 hospitals affiliated with Beth Israel Deaconess Medical Center and Lahey Health, may be nearing final approval from the state. The new, combined entity would approach Partners HealthCare, the state’s largest health care organization, in terms of numbers of patients served.
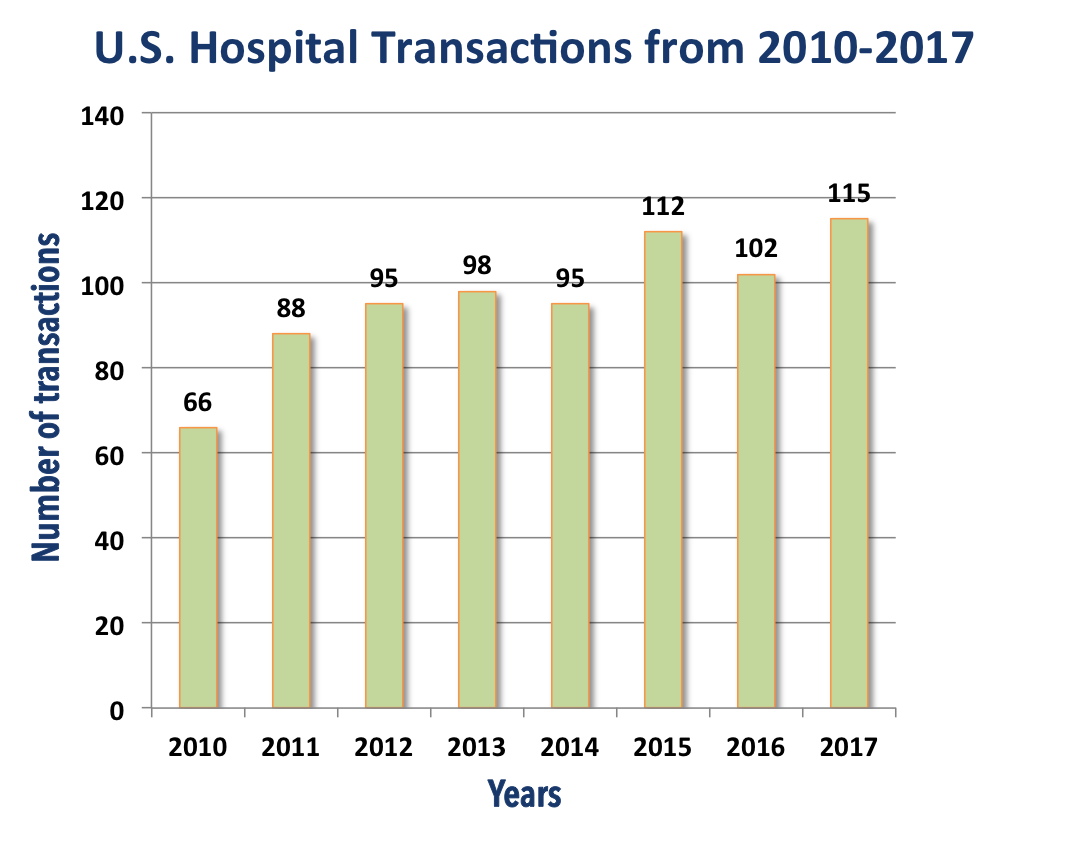
Data source: KaufmanHall
What has driven the hot pace of activity in new partnerships among health organizations? And are quality and safety issues part of those discussions?
“A lot of what is happening these days involves academic medical centers looking for community partners to be able to expand the size of their integrated health systems, looking for new referrals, but also looking to push out to less expensive environments,” explains Mark E. Reynolds, President and CEO of CRICO, which provides insurance and risk management to Harvard’s medical institutions.

But with the increase in mergers and acquisitions, clinical affiliations and physician service agreements comes an important non-financial question. He adds, “We wondered what that would mean for safety.”
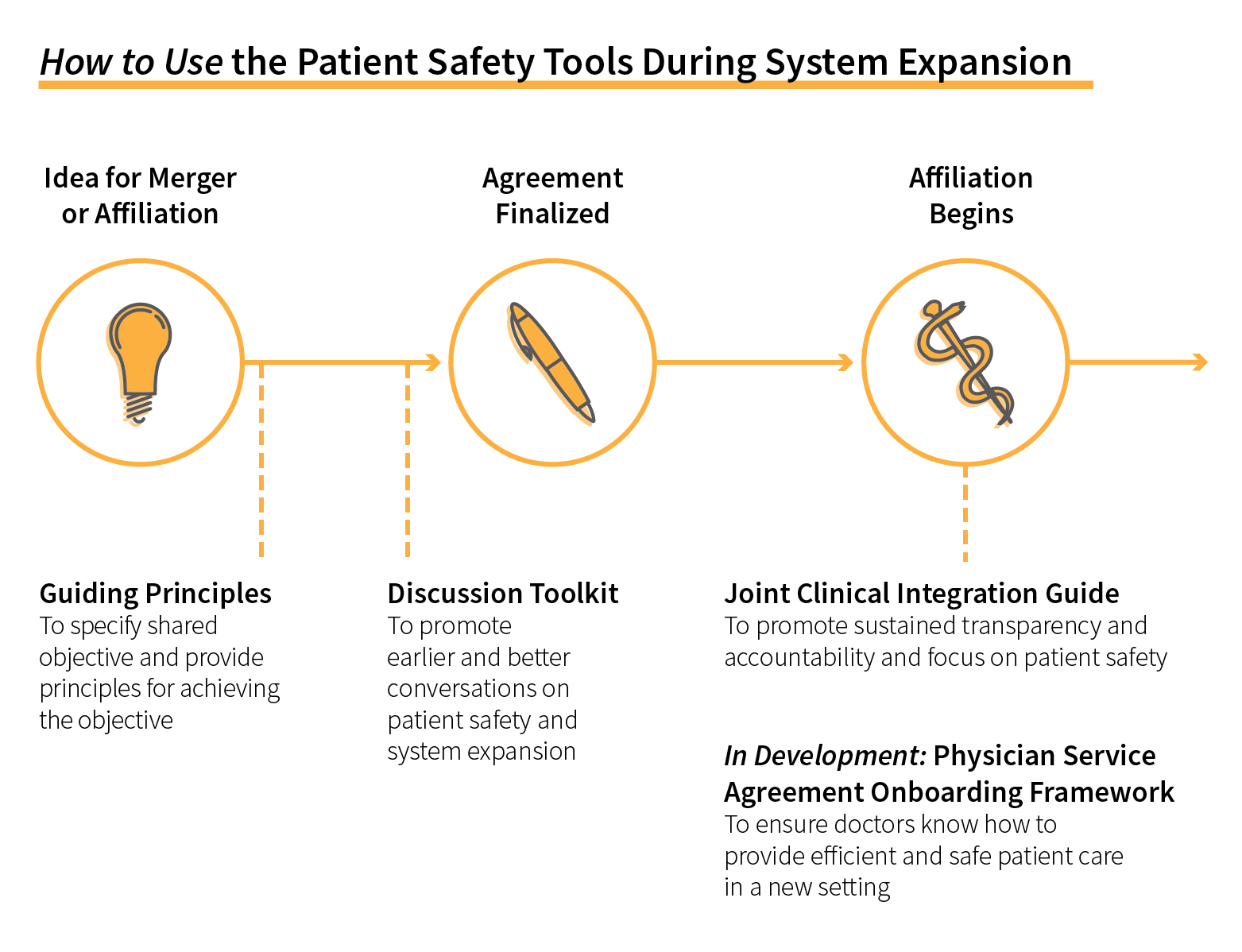
As a result, CRICO teamed up with Ariadne Labs, a Boston-based non-profit to create a toolkit to help clinicians and top administrators uncover important safety considerations and mitigate potential harm before and after the affiliation occurs.
They quickly discovered there was little data to go on.
“We started from anecdotes and insights from physicians and nurses with personal experience that there was a problem related to system expansion,” says Ariadne’s Susan Haas, M.D., the co-principal investigator for the Project on System Expansion Risks to Patient Safety. “Our problem was what was ‘it’? There’s no measurement. The quality measures we use don't capture the impact of affiliations.”
A 2012 report by the Robert Wood Johnson Foundation found that mergers did not always go hand in hand with quality and safety, stating “consolidation without [clinical] integration does not lead to enhanced performance.” That was also true of deals where hospitals purchased independent physician practices.

That was echoed in a 2014 JAMA Viewpoint by Harvard School of Public Health researchers Thomas C. Tsai, M.D., and Ashish K. Jha, M.D.
“When it comes to the delivery of health care, bigger is not always better,” they wrote. “The volume-outcome relationship varies widely across conditions and outcomes, with the largest benefits occurring among a small number of technically difficult surgical interventions.”
The research suggests that consolidation can heighten the need for meaningful data sharing, streamlined care transitions, and engaged leadership that prioritizes quality and works to achieve better care.
These concepts drive efforts by Massachusetts General Hospital to integrate new facilities into its expanding network in Massachusetts and New Hampshire, says Elizabeth Mort, M.D., Senior Vice President of Quality and Safety for the MGH Lawrence Center for Quality and Safety.
“Our approach to due diligence and evaluating a hospital’s attributes has been influenced by these tools,” she says. “Our approach is evolving, and the tools Ariadne Labs has developed are great complements to the more traditional approaches that we had in place.”
She says MGH’s assessment includes reviews of malpractice claims, regulatory reviews, medical and nursing staff metrics, as well as patient experience and safety culture survey results. But the evaluation also involves “talking with senior leaders as well as frontline physicians and nurses, a great way to explore safety culture, from the board to the bedside.”
Emily Aaronson, M.D., an emergency department physician and Assistant Chief Quality Officer at the Lawrence Center, says the toolkit has the potential to be especially helpful in the onboarding process for physicians. “Although the content in medicine is really the same, the process and important procedures can be very different at different institutions,” she says, “Although you may still give aspirin for somebody who is coming in with chest pain anywhere, the process for activating a cath lab can be very different.”
That view is echoed by Claire Seguin, R.N., an Associate Chief Quality Officer at the Lawrence Center, who worked with community hospital leaders to adapt the toolkit initially designed for surgeons to use as part of orientation for all new community hospital physicians. “Any physician coming into a new hospital should understand how you call a code,” she says.
Tools evolve to address the need
The toolkit is growing. Its first offering was a pre-affiliation discussion guide focused on high-risk areas like surgery, obstetrics and emergency medicine. Next came the process of joining together two distinct operating systems.
“Now you’ve signed on … what are the tools, mechanisms, supports that are needed to deal with the problems you’ve identified and to accomplish the clinical integration goals? The conversation should be designed to understand the business we’re in — taking care of patients,” Haas notes.
A JAMA Perspective published in conjunction with the recently completed third year of the project has generated more than 19,000 page views and is among the top five percent of research articles according to Altmetric, which charts social media. As of early October, the toolkit had been downloaded more than 380 times from 37 states and 17 countries.
Haas says the group’s work for the coming year will focus on physician service agreements and creating frameworks for inter-hospital transfers.
“Safety is what it’s all about,” Haas says.
From “Patient Safety for System Expansion” from Ariadne Labs